Opioids in Our Communities
What are Opioids?
Opioids, like fentanyl or morphine, are drugs that can be prescribed to treat pain. Some people use opioids to obtain a high.
For information about Naloxone and Opioid poisoning prevention, please see our Naloxone and Opioid Poisoning Prevention page.
In our catchment area, we monitor and track trends in opioid-related issues in our communities. The following is information related to opioids throughout our catchment area, including our latest Opioid Report.
Deaths from Opioid Overdose
These data refer to all deaths where opioid overdose was a contributing factor in the cause of death. Deaths may have occurred from the use of a single opioid, or from the use of more than one opioid in combination with other medications, drugs, alcohol, etc.
Number of deaths from opioid overdose by year, NWHU catchment area, 2005-2022*
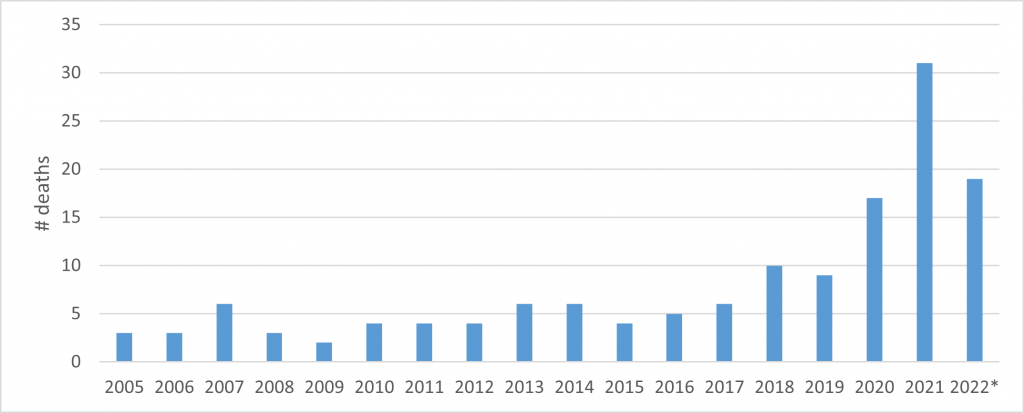
Source: Ontario Agency for Health Protection and Promotion (Public Health Ontario). Interactive Opioid Tool. Toronto, ON: Queen’s Printer for Ontario; 2022. Available from: https://www.publichealthontario.ca/en/dataandanalytics/pages/opioid.aspx
Deaths from opioid overdose per 100,000, NWHU and Ontario, 2005-2022*
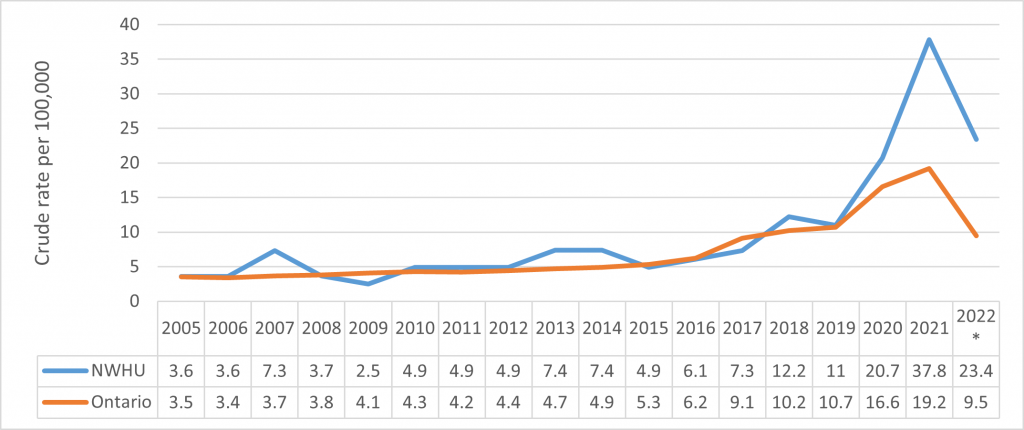
Source: Ontario Agency for Health Protection and Promotion (Public Health Ontario). Interactive Opioid Tool. Toronto, ON: Queen’s Printer for Ontario; 2022. Available from: https://www.publichealthontario.ca/en/dataandanalytics/pages/opioid.aspx
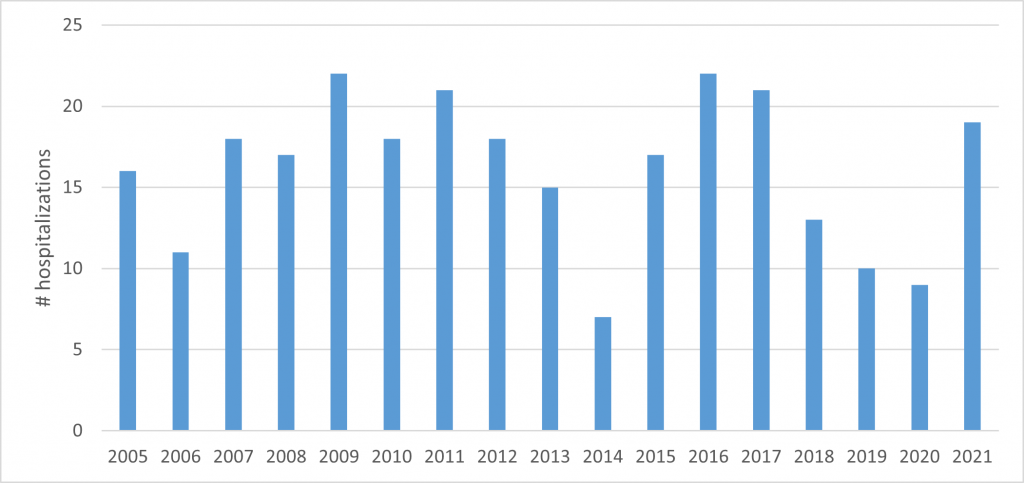
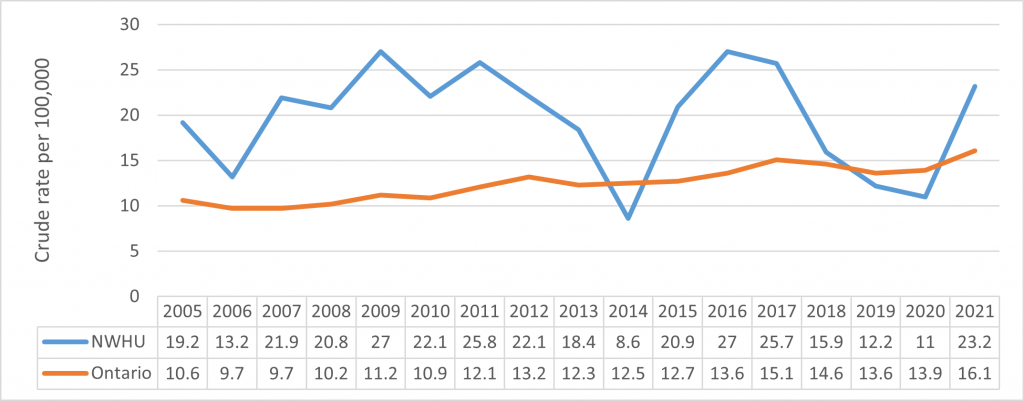
Hospitalizations from Opioid Overdose
These data refer to all hospitalizations where opioid overdose was the main or contributing cause. Not all overdoses result in hospitalization, so these data most likely underrepresent the true volume of overdose in the area. This data source currently has a lag time of approximately 5 months, so the data in this section is not fully up to date with the current situation on overdoses in the NWHU catchment area.
Number of hospitalizations from opioid overdose by year, NWHU catchment area, 2005-2021
Hospitalization from opioid overdose per 100,000, NWHU and Ontario, 2005-2021
Emergency Room (ER) Visits from Opioid Overdose
These data represent all unscheduled emergency room visits where opioid overdose was the main or contributing cause. Not all overdoses result in a visit to the ER, so these data most likely underrepresent the true volume of overdose in the area.
Number of ER visits from opioid overdose by month, NWHU catchment area, 2017-2022*
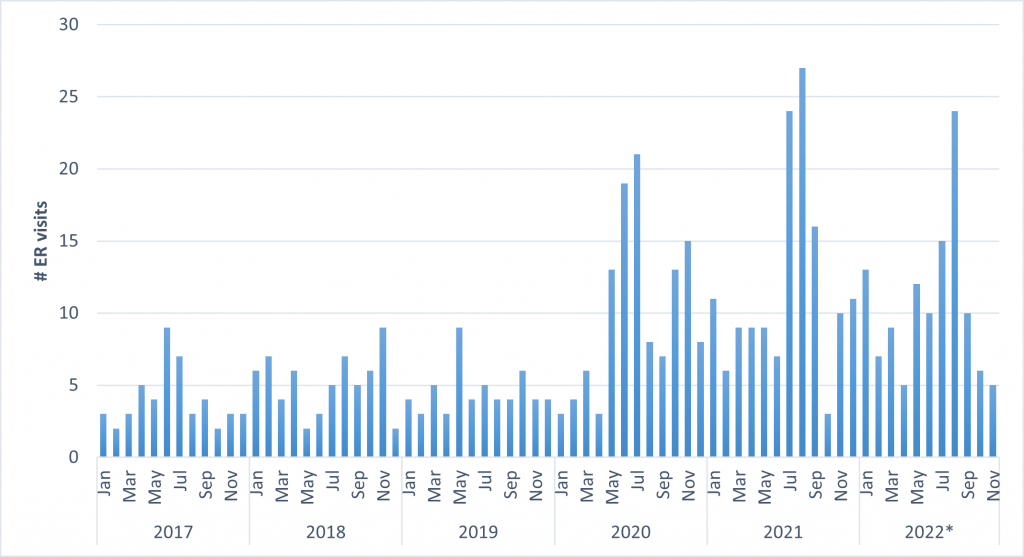
Source: Ontario Agency for Health Protection and Promotion (Public Health Ontario). Interactive Opioid Tool. Toronto, ON: Queen’s Printer for Ontario; 2022. Available from: https://www.publichealthontario.ca/en/dataandanalytics/pages/opioid.aspx
ER visits from opioid overdose per 100,000, NWHU and Ontario, 2005-2022*
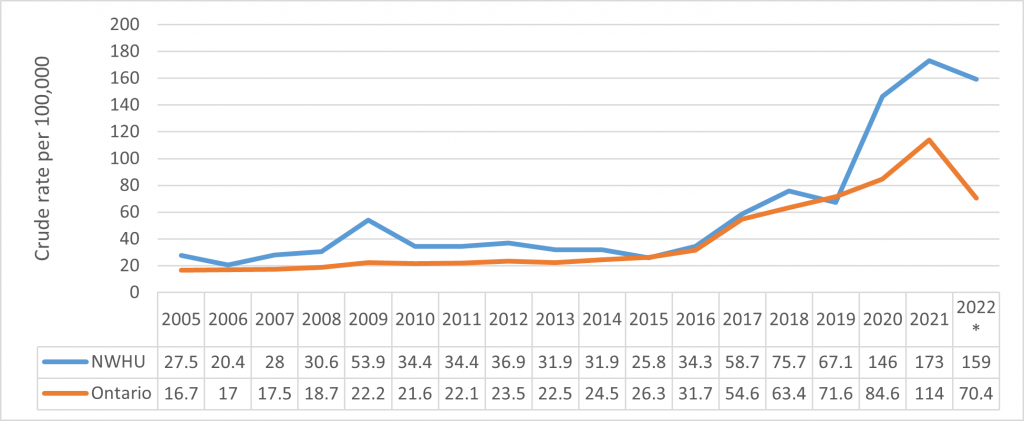
Source: Ontario Agency for Health Protection and Promotion (Public Health Ontario). Interactive Opioid Tool. Toronto, ON: Queen’s Printer for Ontario; 2022. Available from: https://www.publichealthontario.ca/en/dataandanalytics/pages/opioid.aspx
Calls Received by Emergency Medical Services (EMS)
Kenora District
EMS calls where the primary reason was opioid overdose, Kenora District, 2021
| Community | 2021 | 2020 | 2018 | 2017 |
|---|---|---|---|---|
| Dryden | 18 | 12 | 5 | <5 |
| Ear Falls | <5 | <5 | <5 | <5 |
| Ignace | <5 | <5 | <5 | <5 |
| Kenora | 22 | 18 | 11 | 9 |
| Pickle Lake | <5 | <5 | <5 | <5 |
| Red Lake | <5 | <5 | <5 | <5 |
| Sioux Lookout | 9 | <5 | <5 | <5 |
| Sioux Narrows/Nestor Falls | <5 | <5 | <5 | <5 |
| Kenora District Total | 60 | 36 | 23 | 13 |
Rainy River District
EMS calls where the primary reason was opioid overdose, Rainy River District, 2021
| Community | 2021 | 2020 | 2018 | 2017 |
|---|---|---|---|---|
| Atikokan | <5 | <5 | <5 | 0 |
| Emo | <5 | <5 | <5 | 0 |
| Fort Frances | 30 | 24 | 6 | 5 |
| Rainy River | <5 | <5 | <5 | 0 |
| Rainy River District (undesignated) | <5 | <5 | <5 | 0 |
| Rainy River District Total | 37 | 35 | 12 | 5 |
What can you do?
As a community member, I can:
- Receive naloxone training
- Carry Naloxone
- Spend time learning about topics like substance use/addiction and harm reduction from reliable sources
- Think about the language I use when talking about drug use and people who use drugs. Using terms like “person who has an addiction” instead of “junkie” and “addict”
- • Always approach people and situations with compassion and openness
As a service provider, I can:
- Receive training on Naloxone Administration
- Carry Naloxone
- Be mindful of the language I use when talking about drug use and people who use drugs; use terms like “person who has an addiction” instead of “junkie” and “addict”
- Schedule staff presentations on topics relating to harm reduction
- Consider registering my organization as a naloxone distribution site (contact NWHU)
As a person who uses substances, I can:
- Access sterile equipment through harm reduction programs, and never share or reuse drug equipment
- Get trained to use Naloxone
- Carry Naloxone
- Don’t use alone and download the Lifeguard App
- Take part in campaigns/opportunities to destigmatize substance use
- Get familiar with local treatment and support programs
As someone impacted by substance use, I can:
- Learn about local resources
- Access Naloxone
- Access Naloxone training
- Be open and supportive to help friends or family members living with addiction or substance use issues
- Take part in campaigns/opportunities to destigmatize substance use
For more information about Naloxone and Naloxone training, see our Naloxone and Opioid Poisoning Prevention page. If you have any questions or would like more information, please contact your local health unit.