Syphilis Information for Health Care Providers
Syphilis has surged throughout the world including North America and Canada over the past several years, and the NWHU area is included in that trend. Increased testing and prompt access to treatment are crucial to reducing morbidity and mortality related to syphilis. Of particular concern is the increase in congenital syphilis.
Syphilis webinar
Watch our webinar for health care providers on local syphilis information.
Case and contact follow-up for syphilis
100% of syphilis cases reported to NWHU are followed up by a NWHU Public Health Nurse (PHN) who liaises with front line health care providers to facilitate and prompt:
- Early, appropriate antibiotic treatment
- Identification of contacts of the case
- Locating the contacts, and testing of contacts in partnership with primary care providers
- Monitoring subsequent testing
Health care providers who are testing patients for any sexually transmitted or blood-borne infection can improve the outcome by ensuring the patient’s phone number and address are current, accurate, and documented. When the patient is symptomatic or indicating they were a contact of someone with an infection (i.e. high likelihood that the patient is infected), getting as much detail as possible about other sexual contacts or needle-sharing contacts can improve chances of success in getting contacts located, tested, and treated. If public health is made aware of positive test results but cannot locate or connect with the patient, follow-up and contact tracing is often delayed or incomplete, and the spread of disease is less well controlled.
Testing of syphilis
Health care providers should test all clients with any of these risk factors:
- All sexually active individuals with a new or with multiple partners
- If an individual requests STI testing, test for syphilis as well as chlamydia and gonorrhea and any other indicated infections
- All sexually active individuals who continue to have multiple partners should be screened every 3-6 months for syphilis
- Make syphilis testing a norm whenever testing for STIs
Testing while a client is pregnant:
- Our area is experiencing a high rate of syphilis therefore increased screening is indicated
- Pregnant individuals should be tested:
- During the first trimester or at the first prenatal visit
- Repeat testing at 28 to 32 weeks
- Repeat testing at delivery
- Consider screening more frequently pregnant individuals at ongoing risk of infection
- Screen all people who deliver a stillborn infant after 20 weeks of gestation
Health Canada offers a free course for health professionals on barriers to STBBI screening
Treatment of syphilis
First line treatment of syphilis is Long-Acting Benzathine Penicillin G (Bicillin LA). It is important to note this is different from Pen G that can be obtained through normal pharmacy channels. Bicillin LA is a Special Access drug in Canada but can be easily obtained through your local NWHU office.
Clinical Guidelines can be found here: Canadian Guidelines on Sexually Transmitted Infections
More information about treating syphilis includes:
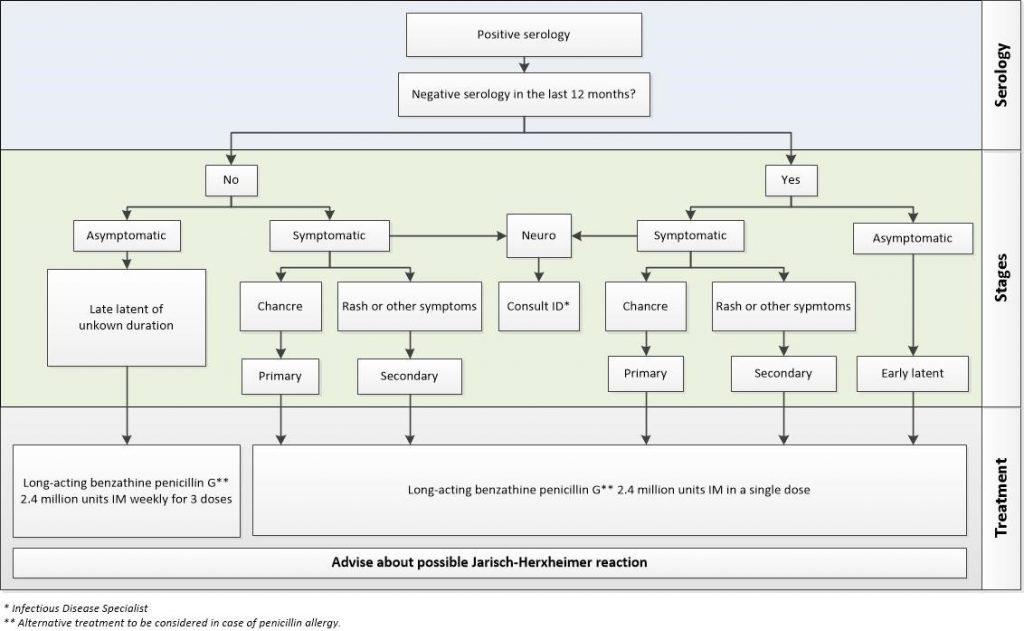
- The number of doses will depend on the stage of the infection
- Excerpt from Canadian Guidelines on Sexually Transmitted Infections:
- Infectious syphilis (primary, secondary and early latent stages): Long-acting Benzathine Penicillin G 2.4 million units intramuscular as a single dose.
- Longer duration syphilis (late latent and tertiary syphilis): Three (3) weekly doses of Benzathine penicillin G-LA 2.4 million units IM.
- Neurosyphilis requires more aggressive treatment with intravenous antibiotics, and should be managed by, or in consultation with, an infectious disease specialist.
- A symptomatic patient is ideally treated at the time of testing to avoid losing contact with the patient and to avoid ongoing transmission
The following excerpt from Syphilis in Canada: Technical report on epidemiological trends, determinants and interventions illustrates sequelae if syphilis is not detected and appropriately or fully treated:
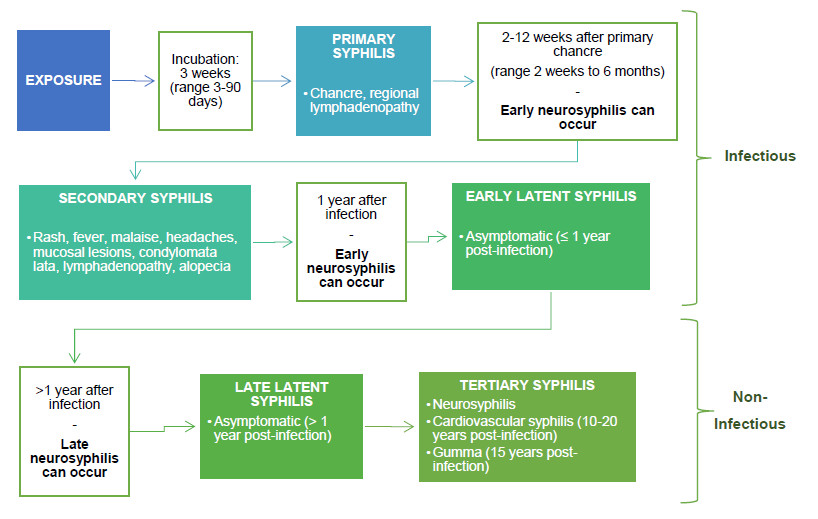
And how to stage a syphilis case:
Prevention of syphilis
Helping to prevent syphilis can include:
- Counsel patients that transmission does not require sexual intercourse and can occur through oral sex or any skin-to-skin contact with a syphilis ulcer that the person may not be aware of
- There is a potential risk related to the sharing of needles
- Condoms and dental dams are available free of charge from the NWHU and can reduce the risk of syphilis and other STI and blood-borne infections
- One-time use needles and other drug-use equipment are available free of charge from the NWHU and can reduce the risk of transmission of syphilis and other blood-borne infections