Tuberculosis (TB) Information for Health Professionals
Tuberculosis (TB) is an ongoing issue throughout northwestern Ontario. Active (infectious) TB disease and Latent TB infection (LTBI) are both reportable diseases in Ontario. Patient consent is not required for reporting this information, and reporting is a legal requirement for healthcare providers as per the Health Protection and Promotion Act.
Health Care Provider roles and responsibilities
The following sections are the roles and responsibilities of a health care provider for both active TB patients as well as latent TB patients.
Active TB Patients
Use the following for active TB patients.
About Active TB
Pulmonary TB is infectious. Active TB can also infect other tissues. Any active TB requires treatment to prevent further deterioration and death. Since active pulmonary TB is an airborne infectious disease, patients are legally required to begin and continue treatment until no longer infectious, so reporting and communicating about new cases is essential.
The annual incidence rate of TB in NWHU’s catchment area (2019-2023) is 6.9 per 100,000. In 2023 there were 8 cases of active TB. The main risk factors are being Indigenous (related to living in a community in which TB has been present in the person’s lifetime) and being born or having lived in a TB-endemic country. You can search specific countries’ TB rates using the World Health Organization’s Tuberculosis profile.
Steps to take for patients with Active TB
| Task | Information |
|---|---|
| Overview |
|
| Detecting | Signs/ symptoms assessment:
Risk factors:
|
| Diagnosing | Diagnostic workup:
|
| Reporting | To report suspected or confirmed active TB:
|
| Contact tracing |
|
| Treatment management and provision of medication |
|
| Infectious Disease Specialist services | Patients with active TB should be managed by a specialist with experience in TB.
|
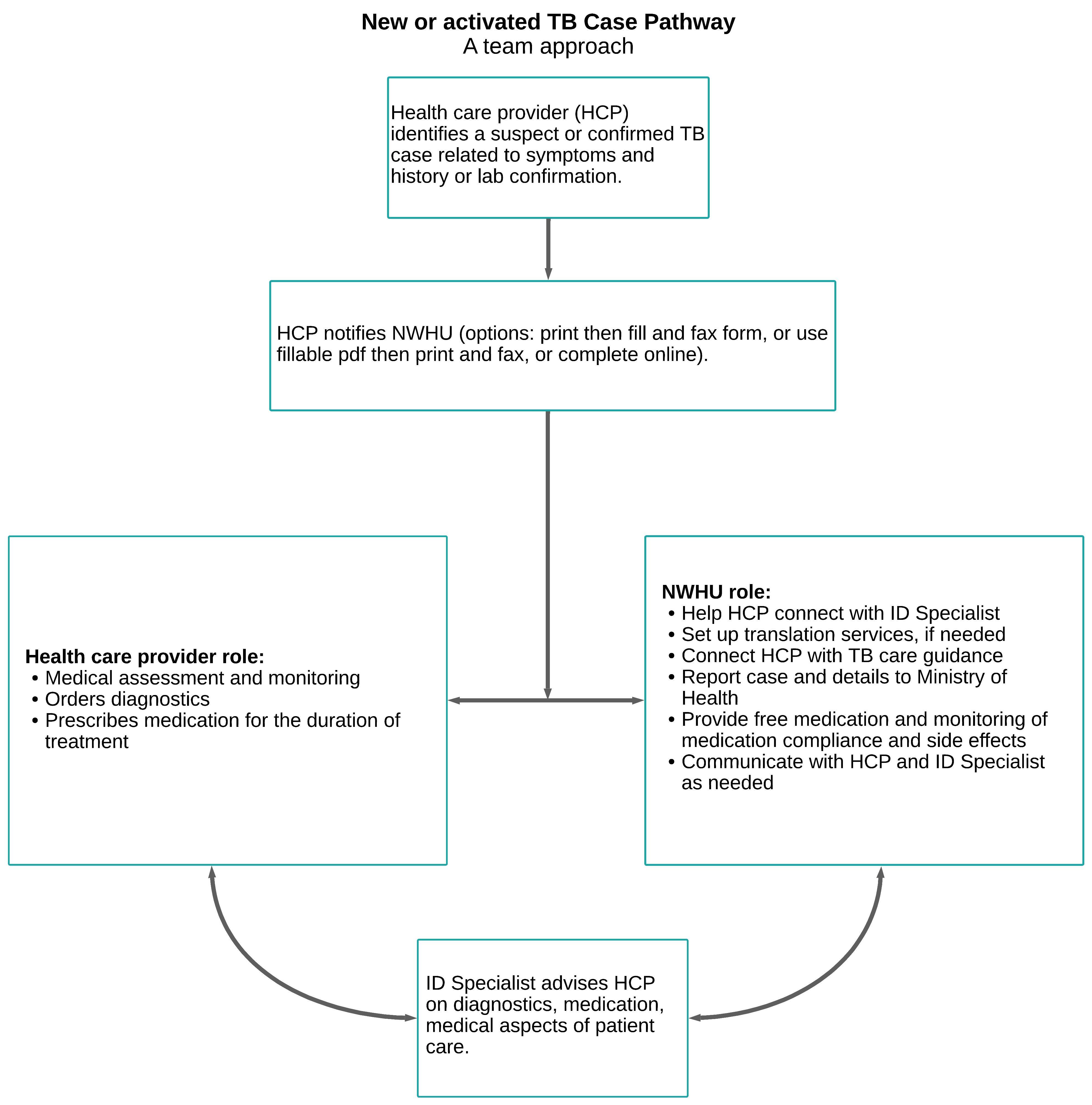
New or activated TB case pathway: A team approach
Latent TB Patients
Use the following for latent TB patients.
About Latent TB
LTBI is not infectious, but reporting LTBI to NWHU is legally required. Patients are not legally obligated to begin or continue treatment because it is not infectious, however, treatment can prevent progression to active, infectious TB. A relationship between the primary care provider and NWHU is important to support the patient in making an informed decision and overall compliance.
NWHU identifies an average of about 33.2 LTBI cases per year (2019-2023). Those who were born or lived in a First Nation or a TB endemic country are most at risk in our region.
Steps to take for patients with Latent TB
| Task | Information |
|---|---|
| Detecting |
|
| Diagnosing |
|
| Reporting | To report a case of Latent TB:
|
| Treatment |
|